![]() Chemical Convulsions and Schizophrenia
Chemical Convulsions and Schizophrenia
![]() The Electroconvulsive Shock Therapy
The Electroconvulsive Shock Therapy
The early decades of the 20th century witnessed a major revolution in the understanding and treatment of mental diseases. Until then, people with psychoses were usually locked away in insane asylums, receiving only limited custodial care and sometimes social support, with practically no effective therapeutic options left to the alienist, as psychiatrists were called then. Although well-intentioned medical reformers such as Phillipe Pinel eased the nightmarish conditions of insane asylums in force well into the first half of the 19th century, no treatments were generally performed. The first revolution was put in motion by scientific psychotherapy, based on theories of the mind proposed by Austrian physician Sigmund Freud, the founder of psychoanalysis. Its value was mainly observable in mild mental disturbances, particularly neuroses. But beginning in the 1930s these methods began to be supplemented by physical approaches using drugs, electroconvulsive therapy, and surgery.
The knowledge that head trauma, convulsions and high fever could be good for improving mental disturbances is not new in Medicine. Hippocrates was the first to note that malaria-induced convulsions in insane patients was able to cure them. In the Middle Ages, some physicians observed the same phenomenon after a severe bout of fever; such as after cholera epidemics in insane asylums. In 1786, a physician named Roess claimed improvement in mental patients after inocculation with smallpox vaccine. Furthermore, many physicans along the centuries have noted that there are very few epileptics who are also schizophrenic, and a biological theory on the incompatibility of convulsions and mental disease slowly evolved. In addition, for centuries physicians had been fascinated with the idea of treating mental and neurological diseases by using electricity.
Between 1917 and 1935, four methods for producing physiological shock were discovered, tested and used in the psychiatric practice, all of them in Europe:
The advent of treatment of the psychoses by using physiological shock increased the opposition between two schools of thought within psychiatry: the psychological and biological ones.
The "psychological school" interpreted mental disease as being due to deviations in the personality, problems in rearing and childhood, discontrol of internal drives, etc. caused by external factors. This school was typified by psychoanalysis, founded by Sigmund Freud in the beginning of the 20th. century.
The "biological school", instead, considered that mental diseases, particularly the psychoses, were caused by pathological alterations of the brain, chemical or structural.
Consequently, the approaches to therapy by each school were markedly different. The success of shock therapy, which was evidently due to some drastic alteration in the internal environment of the brain and on the functions of the neural cells, was a strong argument in favor of the biological causation of many mental diseases.
The first researcher to systematically pursue the link between fever and mental disease was the Austrian physician Julius Wagner von Jauregg. He observed that insane patients improved considerably after surviving to severe typhoid fever, erisipella or tuberculosis infections. Impressed by the coincidence that all of these patients had episodes of high fever and inconscience, he started to do experiments with many methods of inducing fever, such as infection by erisipella, injections of tuberculin, typhoid, etc. without much success.
Wagner-Jauregg's first breakthrough came when he began treating general paresis, a exceedingly severe and common neuropsychiatric disease caused by advanced neurosyphillis, whose cause was unknown at the time. Paresis, also called dementia paralytica, was an incurable and almost always fatal disease, and the insane asylums were full with patients with it, due to the inexistence of effective treatments for syphillis. It was accompanied by marked and progressive neurological and mental degeneration, including convulsions, ataxia (motor incoordination), speech deficits and general and widespread paralysis. Mentally, it caused mania, depression, paranoia and violent behavior, including suicide, delusions, loss of memory, disorientation, and apathy.
The breaktrough was inspired by a startling series of medical discoveries in microbiology, In 1895, Ronald Ross had discovered in India that malaria was caused by a parasite transmitted by the Anopheles mosquito. In 1905, Schaudinn, in Germany, discovered the pathogenic agent for syphillis, the Treponema pallidum. In the same year, Karl Landsteiner proved that fever was able to kill the syphillis-causing spirochetes. In the next year, Wassermann discovered the sorological test for syphillis which is used to detect the infection very early, and in 1908 it was used for the first time for testing the cerebrospinal fluid. In 1909, after 605 attempts at the chemotherapy of syphillis, Paul Ehrlich achieved success with salvarsan or the "606 Compound", on the basis of arsenic, which was the first scientifically designed substance to be used against microbes. Finally, in 1913, Noguchi and Moore demonstrated that general paresis was in fact an infection of the nervous system by syphillis, and this was the first time in medical history that a kind of mental disturbance, or madness, could be traced to a biological alteration of the brain ! The "biological" school of psychiatry had scored a tremendous victory.
Wagner-Jauregg, who was keen in noting every association between fever and paresis, inocculated in July 1917 nine chronic paresis patients with the tainted blood of a malarial soldier. He achieved complete recovery in four ot these patients and an improvement in two more. He then proceeded to devise and to test a complex treatment protocol in 275 syphillitic patients who were at risk for paresis. First he tested their blood and CSF with the Wassermann reaction, then treated them with malarial blood, followed by quinine (to quench malaria) and alternating with injections of neosalvarsan, to clear the blood of spirochetes. His success rate was remarkable: 83 % of the patients were free from the development of paresis. For this, Wagner-Jauregg was awarded the Nobel Prize in 1927.
Nowadays, dementia paralytica is a rare complication of syphillis, and Wagner-Jauregg's treatment has been supplanted by the use of antibiotics.
The second breakthrough in the shock treatment of psychosis was achieved in 1927 by a young Polish neurophysiologist and neuropsychiatrist named Manfred J. Sakel. While an internist in the Lichterfelde Hospital for Mental Diseases, in Berlin, Germany, he provoked a superficial coma in a morphine-addicted woman, using an injection of insulin, and obtained a remarkable recovery of her mental faculties.
Insulin had been discovered in 1921 by two Canadian medical researchers, Frederick Banting and Charles Best, as the hormone fabricated by the pancreas which is responsible for maintaining the equilibrium of glucose in the body. The lack of insulin causes diabetes, or hyperglicemia (excess of glucose), while its natural or artificial excess causes hypoglicemia, which leads to a coma and to convulsions, due to the deficit of glucose in the brain cells.
Sakel's reasoning in using insulin was the following:
"My supposition was that some noxious agent weakened the resilience and the metabolism of the nerve cells ... a reduction in the energy spending of the cell, that is in invoking a minor or greater hibernation in it, by blocking the cell off with insulin will force it to conserve functional energy and store it to be available for the reinforcement of the cell."
Sakel discovered accidentally, by causing convulsions with an overdose of insulin, that the treatment was efficient with patients afflicted with psychosis, particularly schizophrenia. In 1930 he began to perfection what was to become the "Sakel's Technique" for treating schizophrenics, first in Vienna, at the University Neuropsychiatric Clinic, and after 1934, in the United States. The official communication of his technique was made on September 1933, and was enthusiastically received. Until then, no biological treatment for schizophrenia was available. Sakel's approach was a practical and workable physiological method to attack this most debilitating and cruel mental disease. This was to be one the most important contributions ever to be made to psychiatry.
According to his findings, more than 70 % of his patients improved after insulin shock therapy. Two large studies carried out in the USA in 1939 and 1942 gave him fame and helped his technique to rapidly spread out around the world. According to the 1939 study, published for the American Psychiatric Association by John R. Ross and Benjamin Malzberg, among 1757 cases of schizophrenia treated by insulin shock therapy, 11 % had prompt and total recovery, 26.5 % were greatly improved and 26 % had some improvement. The second study, carried out at the Pennsylvania Hospital, had an improvement rate of 63 %, with 42 % of the patients still well after two years of follow-up.
Initial enthusiasm was followed by a decrease in the use of insulin coma therapy, after further controlled studies showed that real cure was not achieved and that improvements were many times temporary. However, since Sakel's method is the gentler and less deleterious of all somatic techniques, it was still in use in many countries until recently.
 In 1933, in the same year that Sakel announced officially his results with the insulin
coma therapy, a young Hungarian physician named Ladislaus von Meduna,
working at the Interacademic Institute of Psychiatric Research, in Budapest, started what would become an entirely
new approach to physiological shock in the treatment of mental disease. Unaware of Sakel's investigations, Meduna
studied the brains and the mental health histories of schizophrenics and epileptics and noted that there seemed
to exist a "biological antagonism" between these two diseases of the brain. Meduna reasoned, then, that
"pure" artificially induced epileptic convulsions could be able to "cure" schizophrenia.
In 1933, in the same year that Sakel announced officially his results with the insulin
coma therapy, a young Hungarian physician named Ladislaus von Meduna,
working at the Interacademic Institute of Psychiatric Research, in Budapest, started what would become an entirely
new approach to physiological shock in the treatment of mental disease. Unaware of Sakel's investigations, Meduna
studied the brains and the mental health histories of schizophrenics and epileptics and noted that there seemed
to exist a "biological antagonism" between these two diseases of the brain. Meduna reasoned, then, that
"pure" artificially induced epileptic convulsions could be able to "cure" schizophrenia.
He then began testing several kinds of convulsant drugs on animals and then on patients. His goal was to achieve completely controllable and reproducible convulsions. The first substance he tested, in 1934, was camphor, but the results were not reliable. He tested also strychnine, thebain, pilocarpin and pentilenetetrazol (also known as metrazol, or cardiazol), always injecting them intramuscularly. Sakel had used many of these drugs together with insulin, in order to enhance the convulsions, but never alone. However, Meduna's aims were achieved only when he experimented with intravenous injections of metrazol. Convulsions ensued quickly and violently, and were dose-dependent. After a series of 110 cases, Meduna could report a discharge rate of 50 %, with remarkable improvements and even "dramatic cures".
Meduna communicated his findings to the psychiatric establishment in a symposium convened at Münsingen, Switzerland, in 1937, to discuss the shock therapy pioneered by Sakel. From this point on, two camps were firmly established in relation to physiological shock therapy: those who defended insulin coma therapy and those who sided with metrazol-induced convulsions. Metrazol was cheaper, much easier to use and more reliable to induce convulsions. Insulin coma required five to nine hours of hospitalization and close follow-up, but it was easily controlled and stopped with injections of glucose or adrenalin, when needed. Metrazol was stronger and more difficult to control. Insulin therapy caused few side effects, while metrazol convulsions were so severe that they caused spine fractures in 42 % of the patients !
Meduna was also forced to immigrate to Chicago, in the USA, in 1939, and from there he continued his research on metrazol convulsions. Eventually, psychiatry recognized that his theory of biological incompatibility between epilepsy and schizophrenia was unfounded, but that artificially-induced convulsions were useful to reduce schizophrenia.
In 1940, A.E. Bennett, a psychiatrist, combined metrazol injections with curare to neutralize the strong muscle contractions which were responsible for this and other incidents. Curare is a muscle paralyzing agent which is extracted from South American plants used by Indians to make poison darts and arrows. It occupies the nerve receptors in muscles, blocking the normal action of acetylcholine neurotransmitter released by motor cells at that point. Later, scopolamine was also used in conjunction with metrazol and curare, to sedate the patient and to avoid the terror of being subjected to violent convulsions while conscient (this was an advantage of insulin).
However, in controlled trials, metrazol seemed to be far less efficient than insulin in the treatment of schizophrenia, particularly chronic disease. It was much more effective in treating the affective psychoses, such as manic-depressive disease and psychotic depression, reaching as much as 80 % of improved patients.
Due to the appearance of many other methods to treat mental disease, including neuroleptics and electroconvulsive therapy, metrazol was gradually discontinued in the late 40's and is no longer in use. It's importance is only historical.

 In 1937, an Italian
neurologist named Ugo
Cerletti was convinced that metrazol-induced
convulsions were useful for the treatment of schizophrenia, but far too dangerous and uncontrollable to be applied
(there was no antidote to stop the convulsions at the time, as it happened with insulin). Furthermore, they were
highly feared by the patients.
In 1937, an Italian
neurologist named Ugo
Cerletti was convinced that metrazol-induced
convulsions were useful for the treatment of schizophrenia, but far too dangerous and uncontrollable to be applied
(there was no antidote to stop the convulsions at the time, as it happened with insulin). Furthermore, they were
highly feared by the patients.
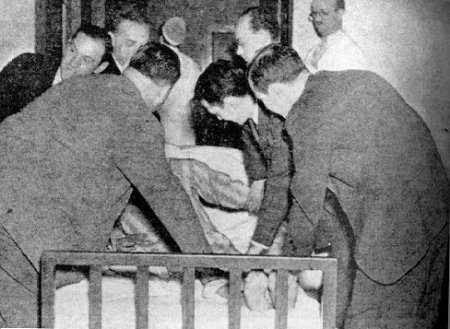
Cerletti knew that an electric shock across the head produced convulsions, because as an specialist in epilepsy, he had done experiments with animals on the neuropathological consequences of repeated epilepsy attacks. In Genoa, and later in Rome, he used a electroshock apparatus to provoke repeatable, reliable epileptic fits in dogs and other animals. The idea to use ECT in humans came first to him by watching pigs being anesthetised with electroshock before being butchered, as a kind of anesthesia, and so he convinced two colleagues, Lucio Bini and L.B. Kalinowski (a young German physician) to help him in developing a method and an apparatus to deliver brief electric shocks to human beings.
They first experimented with several kinds of devices and animals, until determining the ideal parameters and perfecting the technique, and then followed up with a series of electroshocks in human subjects (with acute-onset schizophrenia). After 10 to 20 ECT shocks in alternate days, the improvement in most of the patients were startling. One of the unexpected benefits of transcranial electroshock was that it provoked retrograde amnesia, or a loss of all memory of events immediately anterior to the shock, including its perception. Therefore, the patients had no negative feelings towards the therapy, as it happened with metrazol shock. Furthermore, ECT was more reliable and controllable and less dangerous to the patient than metrazol.
In 1939, Kalinowski began a tour to advertise ECT around the globe, visiting the Netherlands, France, Switzerland, England, and the United States. Researchers who adopted Cerletti-Bini's method soon discovered that it seemed to have spectacular effects on affective disorders. According to E.A. Bennett. 90 % of cases of severe depression which were resistant to all treatments disappeared after three or four weeks of ECT. Soon, curare and scopolamine were being used in conjunction with ECT, and gradually it replaced metrazol and insulin-induced shock. ECT was to begin its long journey as the shock therapy of choice in the majority of hospitals and asylums around the world.
Other kinds of physical shock therapy were briefly tested, such as the induction of fever by means of radiomagnetic microwaves, transient brain anoxia induced by breathing a mixture of oxygen and nitrogen and lowering the body's temperature. Results were mixed, and they were all abandoned in favor of ECT, cheaper and more reliable.
 Significant improvements in the technique of ECT have been made since then, including the use
of synthetic muscle relaxants, such as succinylcholine, the anesthesia of patients with short-acting agents, pre-oxygenation
of the brain, the use of EEG seizure monitoring and better devices and shock waveforms. Despite these advances,
the popularity of ECT greatly decreased in the 1960s and 1970s, due to the use of more effective neuroleptics and
as a result of a strong anti-ECT movement, as we will see below. However, ECT gained evidence again in the last
15 years, due to it's efficacy. It is
the only somatic therapy from the 30's that
remains in widespread use today. Between 100,000 and 150,000 patients are subjected to ECT every year in the
USA, under strictly defined medical conditions.
Significant improvements in the technique of ECT have been made since then, including the use
of synthetic muscle relaxants, such as succinylcholine, the anesthesia of patients with short-acting agents, pre-oxygenation
of the brain, the use of EEG seizure monitoring and better devices and shock waveforms. Despite these advances,
the popularity of ECT greatly decreased in the 1960s and 1970s, due to the use of more effective neuroleptics and
as a result of a strong anti-ECT movement, as we will see below. However, ECT gained evidence again in the last
15 years, due to it's efficacy. It is
the only somatic therapy from the 30's that
remains in widespread use today. Between 100,000 and 150,000 patients are subjected to ECT every year in the
USA, under strictly defined medical conditions.
Many important personalities were subjected to shock therapy. Among them:
Insulin coma therapy: James Forrestal (first US Secretary of Defense, who committed suicide in 1949), Russian ballet dancer Vaslav Nijinski, Zelda Fitzgerald (wife of author Scott Fitzgerald).
Electroconvulsive therapy: writer Ernest Hemingway (who shot himself after undergoing ECT treatment at the Mayo Clinic), poets Silvia Plath (who also committed suicide) and Robert Lowell, performer Paul Robeson, rock star Lou Reed, film actresses Frances Farmer and Gene Tierney, pianists Vladimir Horowitz and Oscar Levant and talk show host Dick Cavett.
 As it happened with psychosurgery, electroconvulsive therapy was a highly troublesome therapy. First, there were many examples
of ECT being used to subdue and to control patients in psychiatric hospitals. Troublesome patients received several
shocks a day, many times without proper restraint or sedation. Medical Historian David J. Rothman affirmed
in an NIH Consensus Conference
on ECT in 1985:
As it happened with psychosurgery, electroconvulsive therapy was a highly troublesome therapy. First, there were many examples
of ECT being used to subdue and to control patients in psychiatric hospitals. Troublesome patients received several
shocks a day, many times without proper restraint or sedation. Medical Historian David J. Rothman affirmed
in an NIH Consensus Conference
on ECT in 1985:
"ECT stands practically alone among the medical/surgical interventions in that misuse was not the goal of curing but of controlling the patients for the benefits of the hospital staff"
However, in the 70's, strong movements against institutionalized psychiatry began in Europe and particularly in the USA. Together with psychosurgery, ECT was denounced by libertarians, and the most famous libel was a 1962 novel written by Ken Casey, based on his experiences on an Oregon mental hospital. Titled "One Flew Over the Cuckoo's Nest", it was later made into a highly successful movie by Czech director Milos Forman, starring Jack Nicholson. Bad press turned into a series of legal actions involving the abuses of shock therapy.
By the mid-1970s ECT had fallen into disrepute. Psychiatrists increasingly made use of powerful new drugs, such as thorazine and other antidepressives and antipsychotics.
See also: Electroconvulsive Shock: Resources on the Internet
 To Know More
To Know More
 The
Author
The
AuthorRenato
M.E. Sabbatini is a neuroscientist
with a PhD in neurophysiology of behavior by the University of São Paulo,
Brasil, and a post-doctoral fellow in the Department of Behavioral Physiology of the Max-Planck Institute of Psychiatry,
Munich, Germany. Currently, Dr. Sabbatini is the director of the Center for Biomedical Informatics and Chairman
of Medical Informatics of the Medical School of the State University of Campinas,
Campinas, Brazil. He is also the associate editor of "Brain & Mind" magazine, and editor-in-chief of Intermedic, a journal on Internet and Medicine.
Email: renato@sabbatini.com