


 Radiosurgery is a procedure which allows non-invasive
brain surgery, i.e., without actually opening the skull, by means of directed
beams of radiation. It is a new technique which is used to destroy, by
means of a precise dosage of radiation, intracranial tumors and other lesions
that could be otherwise inaccessible or inadequate for open surgery. There
are many diseases of the brain for which conventional surgical treatment
is dificult or has many deleterious consequences for the patient, due to
arteries, nerves, and other vital structures being damaged.
Radiosurgery is a procedure which allows non-invasive
brain surgery, i.e., without actually opening the skull, by means of directed
beams of radiation. It is a new technique which is used to destroy, by
means of a precise dosage of radiation, intracranial tumors and other lesions
that could be otherwise inaccessible or inadequate for open surgery. There
are many diseases of the brain for which conventional surgical treatment
is dificult or has many deleterious consequences for the patient, due to
arteries, nerves, and other vital structures being damaged.
Radiosurgeons make use of highly sophisticated, highly precise and complex instruments, such as stereotactic devices, linear accelerators, computers and laser beams. In the last 10 years, radiosurgery has been used as a first approach, by exclusion or failure of other techniques or as supplements to them, such as other kinds of brain surgery, chemotherapy and radiotherapy. The highly precise irradiation of targets within the brain is planned by the surgeon with basis on images, such as computerized tomography, magnetic resonance, and angiography of the brain. The radiation is applied coming from an external source, under precise mechanical orientation by a specialized apparatus. Multiple beams are directed (collimated) and centered at the intracranial lesion to be treated. In this way, healthy tissues around the target are preserved.
 |
 |
 |
 |
 |
|
Computer used for |
Magnetic resonance |
Stereotactic brain atlas |
Stereotactic frame |
Computerized |
Patients can be treated within one day of hospital stay, or even as outpatients. By comparison, the average hospital stay for a craniotomy (conventional neurosurgery, requiring the opening of the skull) is about 16 days. Radiosurgery costs about the same as a conventional surgery, but it avoids mortality, pain and post-surgical complications, such as hemorrhage and infection. The period of recovery is minimal, and in the day following the treatment the patient may return to his or her normal life style, without any discomfort. Thus, the community gains many socio-economical benefits. The major disadvantage of radiosurgery in relation to open surgery (craniotomy) it is the duration of time required to achieve the desired effects, while its non-invasive character is perhaps its major advantage.
Radiosurgery has arisen as the result of many scientific developments which have occurred in the fields of neuroimaging and radiosurgery, continue to expand its application areas in neurosurgery, oncology (cancer), surgery of head and neck, and other specialties.
Radiosurgery started with Dr. Lars Leksell from the Karolinska Institute of Stokholm, Sweden, in the beginning of the 50's, in a joint development with Borje Larsson, from Upsalla University. Leksell used heavy particles, protons from a to irradiate tumor lesions.
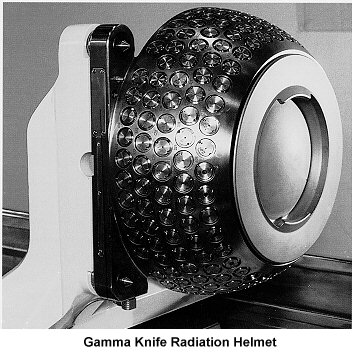 In
the 60's, they developed the "gamma knife", a new device
exclusively for radiosurgery, which consisted of radioactive sources of
Cobalt-60 placed in a kind of helmet with central channels for irradiation.
In the last version of this device, 201 sources of radioactive cobalt direct
gamma radiation to the center of a helmet, where the patient's head is
inserted. i
In
the 60's, they developed the "gamma knife", a new device
exclusively for radiosurgery, which consisted of radioactive sources of
Cobalt-60 placed in a kind of helmet with central channels for irradiation.
In the last version of this device, 201 sources of radioactive cobalt direct
gamma radiation to the center of a helmet, where the patient's head is
inserted. i
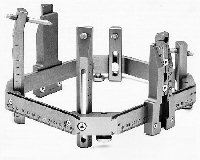 In
order to achieve high precision in the positioning of the patient's head,
it is placed first on a rigid frame of reference called a stereotactic
device. It uses a geometrical coordinate system for each structure
of the brain, so the surgeon knows, by using an a published atlas, precisely
where is the point where the gamma rays must converge. The stereotactic
frame then fits into the helmet.
In
order to achieve high precision in the positioning of the patient's head,
it is placed first on a rigid frame of reference called a stereotactic
device. It uses a geometrical coordinate system for each structure
of the brain, so the surgeon knows, by using an a published atlas, precisely
where is the point where the gamma rays must converge. The stereotactic
frame then fits into the helmet.
The "Gamma-knife" is used nowadays in four continents for carrying out what is called functional stereotactic neurosurgery, and for the superselective irradiation of tumors and arterio-venous malformations.
 Another
type of radiosurgery which has enjoyed great dissemination in neurosurgery
was introduced by Betti and Colombo, in the mid 80's, utilizing commercial
medical linear accelerators available for radiation therapy in oncology
(the so-called Linac).
Another
type of radiosurgery which has enjoyed great dissemination in neurosurgery
was introduced by Betti and Colombo, in the mid 80's, utilizing commercial
medical linear accelerators available for radiation therapy in oncology
(the so-called Linac).
This system differs from the Gamma Knife on the way the radiation beams are delivered to the patient's head. In a similar way, a stereotactic device is used to provide a geometric coordinates reference, but the radiation beams are emitted by a single source, which rotates slowly around the patient's head.
Finally, in advanced medical centers such as in Boston and in California, particle accelerators built for doing research in high energy physics are being used since the 60's for the treatment of brain tumors and AV malformations in humans. A still experimental type of radiosurgery, that utilizes a nuclear reactor for the atomic fission of uranium, is the 'Neutron Therapy Capture' (NCT) which was started in the USA at the nuclear reactor of the Massachussetts Institute of Technology in the 60's, with umpromising results. Nowadays it is carried out as a promising advanced clinical research, due to the progress and to the results obtained in Japan by Dr. Hiroshi Hatanaka. He used NCT in more than 100 cases in the treatment of malignant tumors and of gigantic arterio-venous malformations. In a few years some European, American, and Australian centers shall begin clinical activities with NCT.
The fundamental principle of radiosurgery is that of selective ionization of the tissue to be operated upon, by means of high-energy beams of radiation. Ionization is the production of inorganic ions which are usually deleterious to the cells, by forming free radicals that are harmful to the cellular and nuclear membranes, and even to the RNA and DNA chains of the cells, producing an irreparable damage to these structures and then the cell's death. Thus, biological inactivation is carried out in a volume of tissue to be treated, with a precise destructive effect. The radiation dose absorbed by the treated mass of tissue is what defines the degree of biological inactivation. It usually is measured in units of Gray, the quantity of energy defined by one joule per kg of mass.
In order to perform optimal therapy, the neurosurgeon, assisted by physicists specialized in nuclear medicine, chooses the best type of radiation to be used, and how it will be delivered. Usually, the total dose of radiation required to kill a tumor, for example, is not delivered in a single, massive section, because this would cause collateral, undesirable effects on the patient. Instead, it is divided into several sessions of smaller duration and energy dose, in a procedure called dose fractioning. Even when administered with intervals of several days between them, the ionizing effect accumulates in the tissue. thus achieving the same results with less undesirable consequences for the patient. In order to plan the radiation incidence and dosage, the physicists draw a map portraying the lines of equal intensity of radiation upon the patient's head (this is called a isodose map). Information about the tumor's location is obtained from a series of computerized tomograms, which are then feed to special planning computer software.
There are two types of radiations used in radiosurgery: neutrons and gamma rays.
The first type of radiation is comprised by gamma rays, which are beams of high energy photons that interact with the corona of electrons of the atoms that compose the irradiated tissue, ionizing them. Gamma radiation is used in the "Gamma Knife" device, where they are produced by fixed sources of radioactive cobalt.
 They
are also used in radiosurgery performed in a linear accelerator, the source
being now a commercial medical device of universal use in radiotherapy.
The Linac consists of a emitting tube of gamma radiation, with an energy
of 4, 6, or 18 million electron-volts (MeV).
They
are also used in radiosurgery performed in a linear accelerator, the source
being now a commercial medical device of universal use in radiotherapy.
The Linac consists of a emitting tube of gamma radiation, with an energy
of 4, 6, or 18 million electron-volts (MeV).
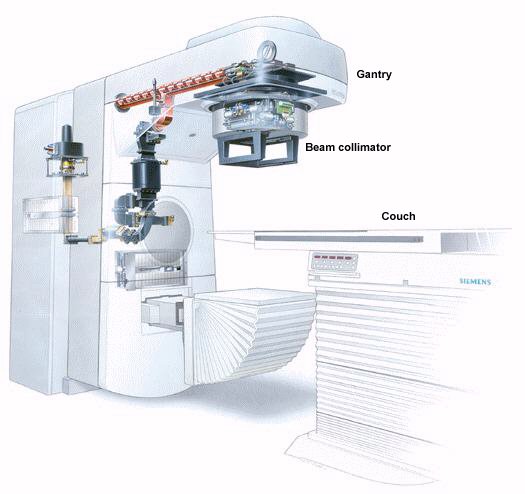
 The
emission head (called "gantry") is mechanically rotated
around the patient , in a full circle. The table where the patient is lying,
the 'couch,' can also be moved in small linear or angular steps. The combination
of the movements of the gantry and of the couch makes possible the computerized
planning of the volume of brain tissue which is going to be irradiated.
Devices with an energy of 6 MeV are the most suitable for the treatment
of the brain, due to the smaller volume to be irradiated. In addition,
the diameter of the energy beam leaving the emission head can be adjusted
to the size of the lesion by means of nterchangeable collimators
(an orifice with different diameters, varying from 5 to 40 mm, in steps
of 5 mm).
The
emission head (called "gantry") is mechanically rotated
around the patient , in a full circle. The table where the patient is lying,
the 'couch,' can also be moved in small linear or angular steps. The combination
of the movements of the gantry and of the couch makes possible the computerized
planning of the volume of brain tissue which is going to be irradiated.
Devices with an energy of 6 MeV are the most suitable for the treatment
of the brain, due to the smaller volume to be irradiated. In addition,
the diameter of the energy beam leaving the emission head can be adjusted
to the size of the lesion by means of nterchangeable collimators
(an orifice with different diameters, varying from 5 to 40 mm, in steps
of 5 mm).
The second type of radiation is used in neutron-capture therapy (NCT).
The process of radiation absorption which happens here is described in
physics as the 'Bragg-peak' effect. A nuclear pile is used to irradiate
the patient's head with heavy neutrons. The neutrons leave the pile through
a special conduit called the "medical port". Arriving at
the target in the brain, the neutrons collide with the nuclei of the target
atoms in the area to be treated. In order to achieve maximum energy, atoms
of boron are used. They are absorbed by the cancerous cells within the
brain, when carried by a special substance which is injected into the patient's
blood circulation. The nuclear fission of boron atoms then releases a number
of protons (called alpha particles), leading to ionization and the death
of the "bad" cells. All this happens within a circle with a radius
of 0.01 mm around fissioned atom, achieving a high degree of ionization
in this region.
 The
selection of the proper kind of radiation and device depends on many factors.
Radiosurgery by Gamma-Knife is applied in isocenters of up to 30 mm of
diameter, which therefore works better for small lesions. Linear accelerators
achieve isocenters of up to 40 mm of diameter. With proton cyclotrons,
the treatable lesions can have up to 100 mm of diameter; while in neutron-capture
therapy, the field can be the whole head.
The
selection of the proper kind of radiation and device depends on many factors.
Radiosurgery by Gamma-Knife is applied in isocenters of up to 30 mm of
diameter, which therefore works better for small lesions. Linear accelerators
achieve isocenters of up to 40 mm of diameter. With proton cyclotrons,
the treatable lesions can have up to 100 mm of diameter; while in neutron-capture
therapy, the field can be the whole head.
 |
Radiosurgery has been specially helpful
for the localized, highly precise treatment of brain tumors. Due to the
steep fall of the irradiation fields (isodoses) from the center of the
target to be destroyed, the biological inactivation happens only on it;
while the brain, and other vascular and neural structures around it, are
protected. This is achieved through the high mechanical precision of the
radiation source, and the assured reproducibility of the target. The precision
in the positioning of the patient, in the calculation of dosages, and in
the safety of the patient, are all extremely high.
Radiosurgery is indicated primarily for the therapy of tumors of the brain and of the hypophysis. These tumors can be primary (i.e., they originated in the brain tissue itself) or metastatical (i.e., they originated from the spread of primary tumors growing in other parts of the body). Radiosurgery works equally well with benign or malignant tumors. |
| The effect of a stereotactic radiosurgery
on a brain tumor Left: before surgery. Right: 4 months after surgery |
The non-interference with the life quality of the patient in the post-operatory period competes with the inconvenience of the latency of months until the result of the radiosurgery is accomplished. Patients with a bad general state of health and those with tumors which are unreachable by conventional means, are specially helped.
The best results become evident three months after the treatment. Usually there is no new growth of tumors in the irradiated region. Radiosurgery has been used to treat many kinds of brain tumors, such as acoustic neuromas, astrocitomas, gliomas, germinomas, meningeomas, among others. Even highly fatal cancerous metastases in the brainstem can be reduced, leaving the patient neurologically intact. It has been demonstrated by the thousands of successfully treated cases, that radiosurgery can be a very safe and efficient method for the management of many difficult brain lesions, while it avoids the loss in quality of life associated to other more invasive methods. Patients are being treated for lesions which only radiosurgery can solve, or because they prefer it as a first treatment, after receiving complete information of its risks and benefits as compared to the conventional surgery, when the choice is available.
In the future, advanced computer methods, such as virtual reality,
will be used to improve the accuracy and scope of radiosurgery. In the
picture at right, a 3D reconstructed image of the tumor is visualized by
the neurosurgeon, using special 3D goggles, as a projection onto the patient's
head, with precise conservation of the spatial relations of one in relation
to the other.
 To
Know More
To
Know More
Copyright (c) 1997 State University of Campinas, Brazil